Chronic Kidney Disease (CKD) is a severe and progressively debilitating condition affecting millions globally. As it progresses, CKD can drastically impair kidney function, which threatens overall health. Thankfully, contemporary medical advancements provide effective treatments to manage CKD efficiently.
Two reliable methods to enhance the quality of life for CKD patients are dialysis and kidney transplantation. In this post, we will delve into these advanced treatments, examining their mechanisms, advantages, and considerations for those living with CKD.
Understanding Chronic Kidney Disease
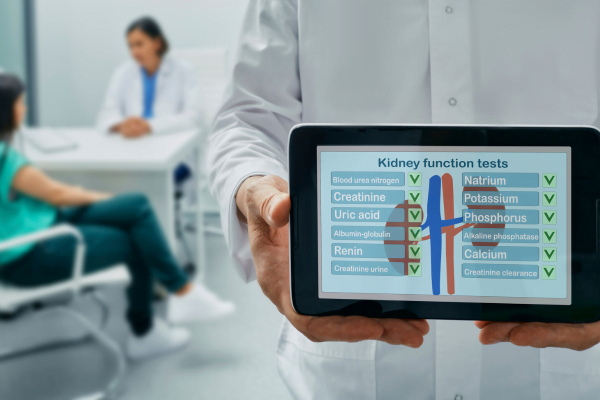
Before exploring treatment options, it’s essential to understand the fundamentals of Chronic Kidney Disease (CKD). Kidneys play a crucial role in filtering waste products and excess fluids from the bloodstream, maintaining electrolyte balance, and producing essential hormones. As CKD progresses, these vital functions decline, leading to the accumulation of waste and fluids in the body. It’s worth noting that the human body typically possesses two kidneys.
Stages of Chronic Kidney Disease
CKD is categorized into five stages based on the glomerular filtration rate (GFR), indicating the kidneys’ filtering efficiency. In the early stages, patients may not notice symptoms. However, as the disease progresses, symptoms such as fatigue, swelling, and changes in urine output become more evident.
Advanced Treatment Options
Dialysis
Dialysis is a crucial medical procedure that mimics kidney functions by removing wastes and excess fluids from the body. There are two main types: hemodialysis and peritoneal dialysis.
**Hemodialysis:** This procedure uses an artificial kidney (dialyzer) to filter blood outside the body. Blood is drawn, filtered through the dialyzer, and returned to the body. Typically, this process occurs at a dialysis center three times a week, each session lasting several hours.
**Peritoneal Dialysis:** In this method, the peritoneum (a membrane lining the abdominal cavity) acts as a natural filter. A cleansing solution is introduced into the abdomen via a catheter, and waste products pass from blood vessels into the solution. After a dwell time, the solution carrying the waste is drained from the body. Peritoneal dialysis can be performed at home, providing more flexibility for patients.
Benefits of Dialysis
Dialysis is vital for maintaining health in advanced CKD. Key benefits include:
**Waste Removal:** It helps eliminate waste products and excess fluids, preventing harmful toxin buildup.
**Fluid Balance:** Dialysis regulates fluid levels, managing blood pressure and reducing complications related to fluid retention.
**Symptom Relief:** It can relieve symptoms such as fatigue, nausea, and shortness of breath associated with advanced CKD.
Considerations for Dialysis Patients
Patients on dialysis should consider the following:
**Lifestyle Changes:** Regular sessions demand a commitment and may impact daily routines, necessitating adjustments.
**Dietary Restrictions:** Kidney-friendly diets are crucial, with potential limitations on certain foods and fluids to manage electrolyte balance.
**Access to Care:** Hemodialysis requires attendance at specialized centers, meaning reliable transportation and healthcare access are essential.
Kidney Transplantation
Kidney transplantation is the gold standard for treating end-stage renal disease (ESRD) when kidney function is severely impaired. This procedure involves transplanting a healthy kidney from a living or deceased donor into the recipient, restoring kidney function.
**Living Donor Transplants:** Transplants from living donors, often family or friends, offer benefits such as shorter waiting times and potentially better outcomes.
**Deceased Donor Transplants:** These transplants involve kidneys sourced from registered organ donors or those whose families donated their organs after death.
Benefits of Kidney Transplantation
Improved Quality of Life
Kidney transplantation significantly improves the quality of life compared to dialysis, allowing for greater normalcy and fewer restrictions. While dialysis imposes strict dietary and fluid limitations, a successful transplant restores the body’s ability to filter waste efficiently, enabling a more flexible lifestyle. Additionally, patients report higher energy levels, improved mental well-being, and a sense of freedom from chronic illness constraints, positively impacting relationships and overall satisfaction.
Long-term Solution
While dialysis requires a lifelong commitment, a kidney transplant offers a more enduring solution to CKD. Post-transplant care primarily involves medications and regular checkups, which are less demanding than continuous dialysis sessions. This transition allows for a return to normalcy and independence. Furthermore, successful transplants significantly extend and improve life expectancy, offering years of enhanced health.
Better Health Outcomes
Studies consistently show that kidney transplantation leads to better health outcomes than long-term dialysis, reducing complications associated with CKD. Transplant recipients generally have lower mortality rates and fewer heart problems, infections, and other dialysis-related complications due to restored normal kidney function, promoting overall physiological balance.
Considerations for Transplant Recipients
Transplant recipients need to consider:
**Immunosuppressive Medications:** Lifelong use of these drugs is necessary to prevent organ rejection, with potential side effects and the need for close monitoring.
**Organ Rejection:** Despite medical advancements, organ rejection remains a risk; regular follow-up and adherence to medication regimens are crucial.
**Donor Compatibility:** Finding a suitable donor is vital for transplant success, requiring compatibility tests to reduce rejection risk.
Bottom Line
In summary, advanced treatments such as dialysis and kidney transplantation significantly impact CKD patients’ lives. While dialysis effectively manages symptoms and improves well-being, kidney transplantation offers a more permanent solution, enhancing quality of life and extending lifespan. Patients and healthcare providers should carefully evaluate each option’s pros and cons to determine the most appropriate treatment approach.
FAQ
When is dialysis needed?
Dialysis is necessary when kidneys can no longer filter waste products and excess fluids effectively due to advanced kidney disease or failure. It maintains electrolyte balance and manages blood pressure, ensuring overall health.
How long can someone live on dialysis?
Life expectancy on dialysis varies, with an average survival rate of 5 to 10 years, though some live longer with proper care. Factors such as overall health, age, treatment adherence, underlying conditions, and access to kidney transplantation influence longevity.